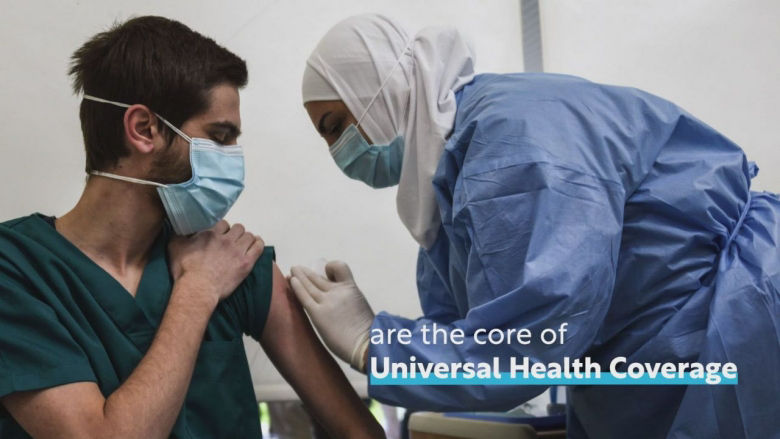
Universal health coverage (UHC) is about ensuring that everyone, especially the most vulnerable, has access to the quality health care they need without suffering financial hardship. It is key to achieving the World Bank’s mission to end extreme poverty and boost prosperity on a livable planet, and it is the driving force behind all of the WBG’s health and nutrition investments.
UHC allows countries to make the most of their strongest asset: human capital. Supporting health represents a foundational investment in human capital and in economic growth—with good health, children can attend school and eventually reach their full potential, while adults are able to lead productive healthy lives.
Global movement towards UHC
Universal health coverage is an important part of the Sustainable Development Goals (SDGs). SDG 3.8 aims to “achieve universal health coverage, including financial risk protection, access to quality essential health care services, and access to safe, effective, quality, and affordable essential medicines and vaccines for all.” In addition, the SDG 1 call to “end poverty in all its forms everywhere” could be in peril without UHC given that out-of-pocket health spending pushes people into, or further into, poverty.
The UHC movement has gained global momentum. In September 2023, the United Nations adopted a high-level political declaration to reaffirm and renew commitment to UHC in a post-COVID world. However, turning commitment into reality will require new ways of working to overcome challenges.

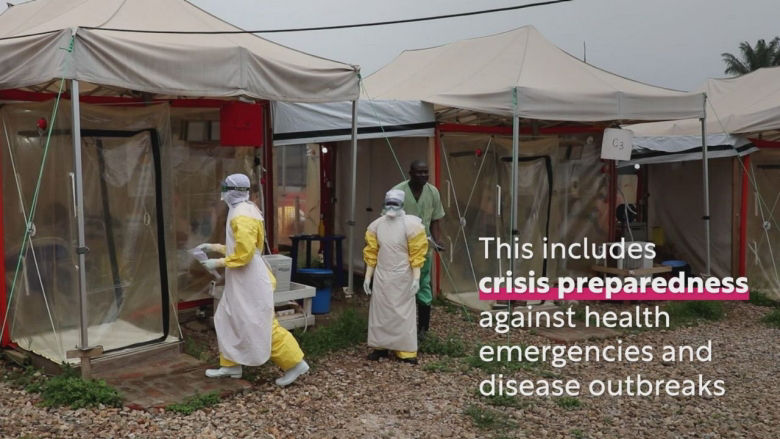
Intertwined challenges
Half of the world’s population -or 4.5 billion people- is not covered by essential health services, and 2 billion people face severe financial hardship |
Since 2015, health service coverage has stagnated and financial hardship due to out-of-pocket health spending has worsened, undermining efforts to eradicate poverty globally.
Global commitments for women, children and adolescents are falling behind.

Demographics and disease profile are changing and put pressure on health systems. Globally, fertility has fallen significantly from an average of 5 births per woman in 1950 to 2.3 per woman in 2021.
Populations are also aging worldwide: people aged 65 and older now outnumber children under 5. By 2050, 1.5 billion people will be 65 and older. Non-communicable diseases (NCDs) are on the rise, accounting for 41 million deaths each year (74% of all deaths globally), with more than three quarters of NCD deaths occurring in low and middle-income countries.
Climate change is also a critical contributor to the burden of NCDs through factors such as air pollution, heat stress, and extreme weather events.
At the same time, the lack of countries’ health service capacity hinders progress on mental illnesses. More than three quarters of people with a severe mental disorder are not receiving treatment in low and middle income.
These shifts require health systems to adapt to be greater responsive to changing needs of the population, but such changes also have implications for the financing of health systems.
Health is an investment, not an expense
Last Updated: Dec 12, 2024