Addis Ababa, November 18, 2024—“I have lived with HIV my whole life, but it’s not HIV that I am worried about,” says Brandon Jaka from Zimbabwe, “It’s what follows, when medicines that are supposed to treat infections fail to do so.” Brandon is part of the World Health Organization’s (WHO) taskforce of Antimicrobial Resistance survivors, and you can watch his story here.
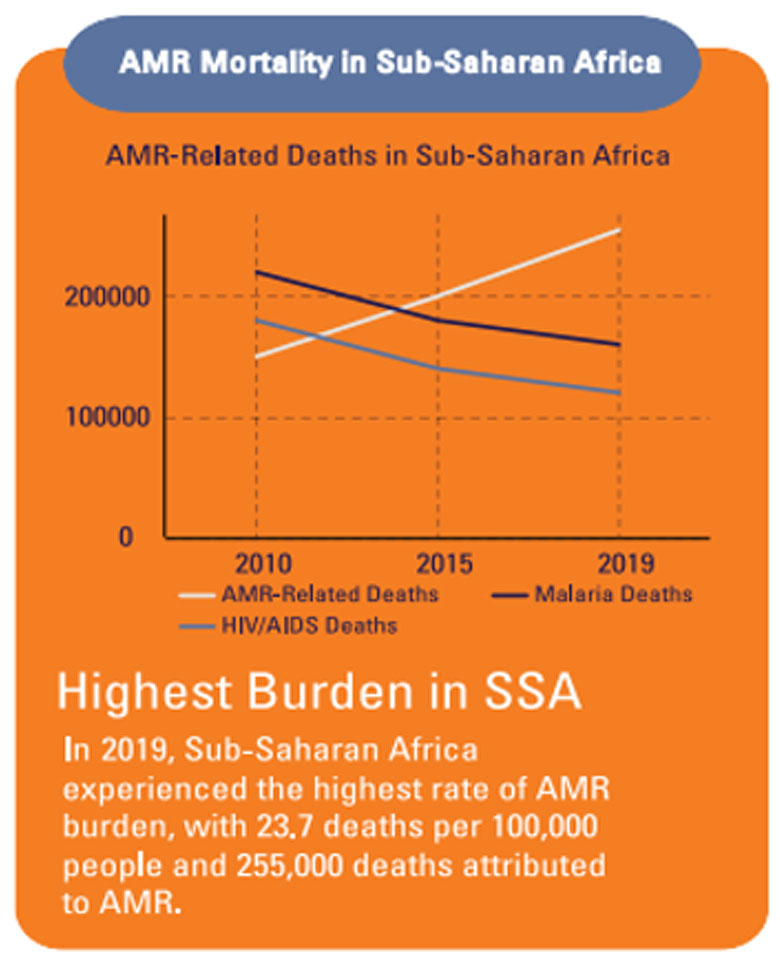
Antimicrobial Resistance (AMR), according to the WHO, occurs when bacteria, viruses, fungi and parasites no longer respond to antimicrobial medicines, mainly due to the misuse and overuse of antimicrobials to treat, prevent, or control infections in humans, animals, and plants. AMR is a silent but serious global health emergency. In Africa, it has now become a significant cause of mortality, with deaths from infectious diseases such as malaria, HIV, and tuberculosis being largely caused by drug-resistant strains of these diseases.
What causes AMR? The careless use of antimicrobials is a definite part of the cause, but in Africa, a lack of access to clean water, sanitation, and vaccination are also contributory factors. The African Union’s AMR Landmark Report estimates that investments in water, sanitation and hygiene, infection prevention, and biosecurity could save 700,000 lives a year on the continent.
Source: African Union AMR Landmark Report, 2024
The need for coordinated action
African countries are committed to tackling AMR, but translating the AU Framework for AMR Control (2020-2025) into action requires strong coordination across sectors and countries. This is important because AMR cuts across human, animal, and environmental health and requires effective national and regional regulatory frameworks for medicines.
World Bank investments to combat AMR
The World Bank has invested in One Health and specifically in AMR efforts for more than a decade, and is working to support governments in designing and implementing approaches to preserve antimicrobials with financing and technical assistance. Our new Framework for Action helps World Bank teams and clients in designing interventions that address AMR, with a focus on low- and middle-income countries (LMICs), which stand to be disproportionately impacted. This Framework outlines 20 intervention areas across the health, agriculture, and water sectors that can serve as starting points for discussions to develop sustainable systems addressing AMR at the national and regional levels.
Established in the aftermath of the 2014-2016 Ebola outbreak in West Africa, the Regional Disease Surveillance Systems Enhancement (REDISSE) Program engaged 16 countries in West and Central Africa and is benefiting almost half a billion people through a total financing of US$ 670.13 million. This program was instrumental in supporting countries to establish One Health platforms which were critical to bring together human, animal, and environmental health and set forth integrated planning for AMR.
Today, two new regional programs include significant investments in AMR, among other health emergencies faced by African countries. The $1.5 billion Health Emergency Preparedness, Response, and Resilience (HEPRR) Program covers eight countries so far in Eastern and Southern Africa (Burundi, the Democratic Republic of Cong (DRC), Ethiopia, Kenya, Malawi, Rwanda, Sao Tome & Principe, and Zambia), while the $500 million Health Security Program covers three countries in West and Central Africa (Cabo Verde, Guinea, and Liberia). Regional organizations also receive financing under these programs. The Global Financing Facility and the Pandemic Fund provide some co-financing at the country level.