Nearly two decades ago, many low- and middle-income countries began a transformation in health care financing. Centralized budgets and low levels of autonomy for facilities and workers were replaced with frontline autonomy, performance pay, and greater transparency and accountability for results, all through a package of reforms that came to be known as performance-based financing. Unfortunately, while health coverage did expand dramatically over the past two decades, this expansion was not accompanied by the expected improvements in health outcomes.
A new World Bank Policy Research Report, Improving Effective Coverage in Health: Do Financial Incentives Work?, draws on research from 15 years and 40 countries to better understand the gap between health coverage and outcomes and point a way forward. At a Policy Research Talk last month, lead authors Damien de Walque and Eeshani Kandpal, economists at the World Bank, shared key insights from their review of the evidence and recommended a new tack in health financing policy.
“The big picture motivation behind this report is a frustrating status quo,” said de Walque. “Most deaths in low-income countries are due to poor quality care rather than the lack of access to care.”
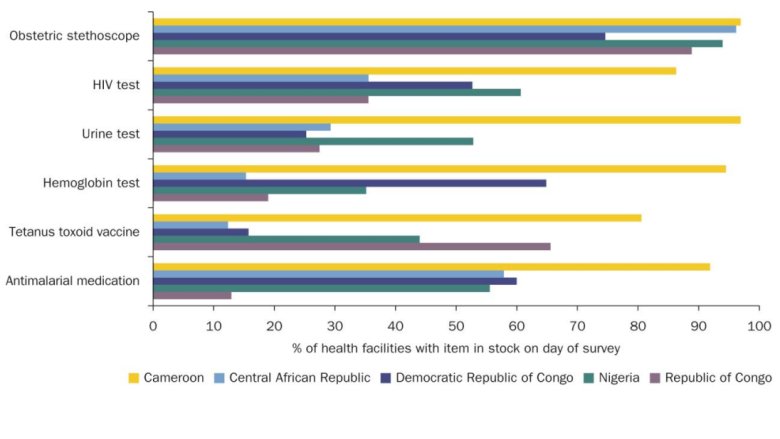
To understand the drivers behind this reality, the authors used a metric called effective health coverage, which measures primary health coverage with a minimum content and quality of care. The data show that the gap between coverage and effective coverage can be extreme. For example, coverage for antenatal care in a number of sub-Saharan African countries is high, but quality is often lacking (Figure 1). In the Democratic Republic of Congo, coverage for antenatal care is around 90 percent, but in fewer than 30 percent of cases does care meet minimum quality standards.
Figure 1: Coverage versus Quality of Antenatal Care
Note: Coverage: percent of women giving birth who had 1+ antenatal care visits. Quality: of those covered, the percent who had 4+ visits, 1+ visits with a skilled provider, blood pressure taken, and blood and urine samples taken (correct treatment). EC = effective coverage. The isoquant lines demarcate comparable levels of effective coverage. See page 21 in the report for more details.
In many low- and lower-middle-income countries (LMICs), the disparity between coverage and quality means that maternal deaths remain unacceptably high, despite widespread access to antenatal care. A study of maternal deaths in 137 LMICs found that of an estimated 207,000 excess deaths in 2016, 57,000 were likely due to poor quality of care, compared to an estimated 47,000 deaths that were due to lack of access to care. This type of pattern holds not only for maternal health but many other health outcomes.
The rollout of performance-based financing (PBF) reforms—which combined performance pay for workers, decentralized frontline financing, transparency and accountability, and community engagement—was intended to address these types of poor outcomes. But according to Kandpal and de Walque, while PBF achieved better outcomes than business-as-usual in low-income settings, the relative benefits of PBF compared to other approaches are less clear. In particular, performance pay to incentivize worker effort proved to only marginally improve outcomes while being costly to implement and monitor. In fact, in one case, verifying performance pay alone consumed two thirds of project administrative costs.
“In trying to improve quality, the first step is to understand what the constraints to quality are,” said Kandpal. “Effective policies need to address not only worker effort, but other factors like structural capacities and medical training.”
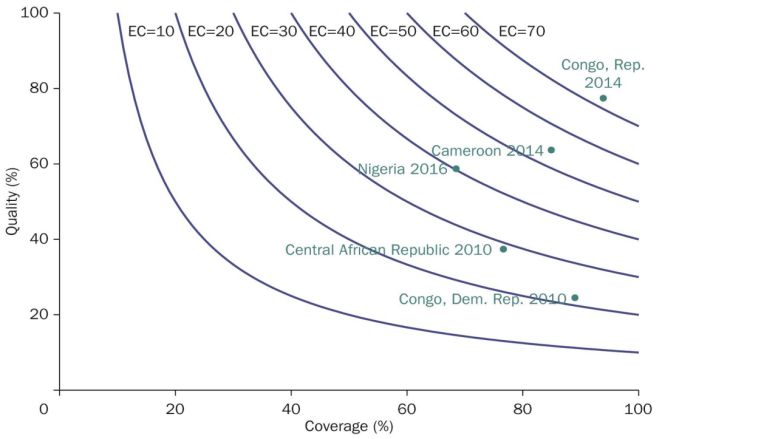
To identify the relative importance of various constraints, the report relies on a “know-can-do” framework that examines structural gaps (e.g., do health care facilities have drugs and equipment in stock?), knowledge gaps (e.g., have health care workers received adequate training to know the correct treatment in a situation?), and gaps in worker effort. The authors found that two thirds of poor quality care cannot be attributed to low worker effort, suggesting that performance pay alone would have limited impact—unsurprising, given the high percentage of health facilities that lack even basic supplies (Figure 2).
Figure 2: Structural Capacity Gaps
Note: See Figure 4.2 on page 66 of the report for more data on structural capacity gaps.
de Walque and Kandpal pointed to alternative approaches to health financing reform as promising models. In particular, Direct Facility Financing (DFF)—which includes decentralized budgeting, light-touch accountability, and community engagement, but leaves out performance pay—has proven effective in a range of low-income settings. Demand-side interventions like vouchers and cash transfers to households can also be effective complements to DFF where patient demand is low.
Zooming out, the researchers concluded with a few key principles for effective health care financing reform. First, they recommend that policy makers assess not only coverage but also effective coverage to ensure they are addressing the most critical gaps in care. Second, before introducing performance pay as part of a reform package, policy makers should identify whether the constraints within a health care system are within the control of frontline health care workers or lie elsewhere. Third, the sequencing of interventions is key: de Walque and Kandpal recommend 18 – 24 months of DFF and demand-side interventions followed by a diagnostics exercise to assess progress before introducing performance pay.